Aortic valve replacement surgery is a vital procedure designed to restore normal heart function in patients with severe aortic valve disease, such as aortic stenosis or regurgitation.
What is Aortic valve replacement?
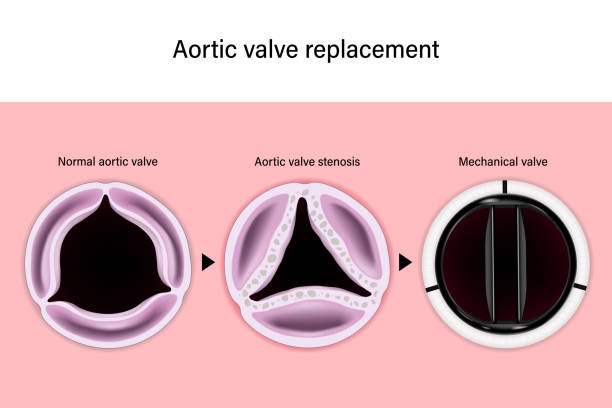
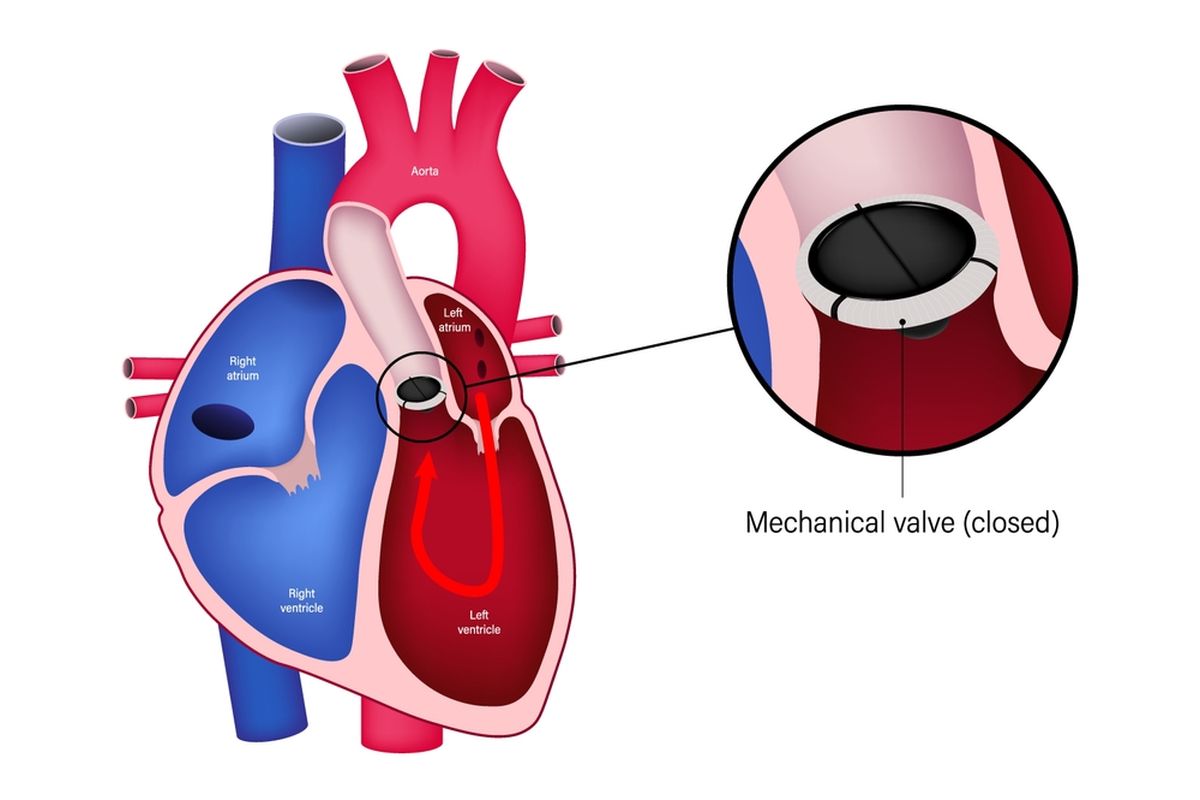
Aortic valvereplacement is a surgical procedure performed to restore proper function to the aortic valve of the heart. The aortic valve is a critical component that controls the flow of oxygen-rich blood from the left ventricle to the aorta and onward to the rest of the body. When this valve becomes diseased or damaged – due to conditions such as aortic stenosis, where the valve narrows, or aortic regurgitation, where it leaks – the heart must work harder, potentially leading to various symptoms like chest pain, fatigue, and shortness of breath. In aorticvalve replacement, the malfunctioning valve is removed and substituted with a prosthetic valve. Options for replacement include mechanical valves, which are durable but require lifelong blood-thinning medication, or bioprosthetic valves, made from animal tissue, which may have a shorter lifespan but typically do not need prolonged anticoagulant therapy. Traditionally, the procedure is performed through open-heart surgery, necessitating a sternotomy and the use of a heart-lung machine to maintain circulation during the operation. However, less invasive techniques such as transcatheter aortic valve replacement have gained popularity for patients who are at higher surgical risk, offering a faster recovery while still effectively relieving symptoms and restoring healthier heart function.
Why would I need a valve replacement?
Valve replacement may be necessary when the heart's natural valves—responsible for maintaining proper blood flow—become significantly impaired by disease, damage, or congenital abnormalities. For many patients, conditions such as aortic stenosis (narrowing of the valve) or aortic regurgitation (leaky closure) place an excessive workload on the heart, leading to symptoms like chest pain, fatigue, difficulty breathing, and fluid buildup. Over time, these issues can cause the heart’s performance to deteriorate, increasing the risk of heart failure. In some cases, valve damage can occur due to infections like endocarditis, or because of structural imperfections present from birth that progressively worsen. When the valve's function becomes compromised to the point where it can no longer efficiently regulate blood flow, a valve replacement becomes a necessary intervention to restore normal heart function and improve overall quality of life. This surgical option not only alleviates debilitating symptoms but also aims to prevent further cardiac deterioration and life-threatening complications. The decision to replace a valve is made after comprehensive cardiovascular assessments and careful evaluation of the patient’s symptoms, medical history, and overall health status.
When is Aortic valve replacement surgery needed?
Aortic valve replacement surgery becomes necessary when the aortic valve, which plays a crucial role in regulating blood flow from the heart to the body, fails to function effectively due to disease or damage. Typically, severe aortic stenosis, characterized by a narrowing of the valve opening, or significant aortic regurgitation, where the valve does not close properly leading to blood backflow, are the primary conditions that necessitate surgery. As these conditions progress, the heart must work harder, ultimately leading to symptoms such as chest pain, shortness of breath, fatigue, and dizziness. In advanced cases, individuals may develop heart failure or experience arrhythmias, further compromising cardiovascular health. Diagnostic tests, including echocardiograms and cardiac catheterizations, allow physicians to assess the severity of the valve dysfunction and gauge the impact on heart performance. When medical management and lifestyle modifications are no longer sufficient in controlling symptoms or preventing further deterioration of the heart muscle, valve replacement becomes the definitive treatment to restore optimal blood flow and improve quality of life.
What are the risks of Aortic valve replacement?
Aortic valve replacement is a critical procedure that comes with inherent risks, which must be weighed carefully against the benefits.
One of the primary concerns is the potential for infection, particularly at the incision site or within the heart, which can extend recovery time and complicate the patient’s overall health.
Bleeding and blood clot formation are also risks, with clots possibly leading to stroke or additional cardiovascular events.
The use of a heart-lung machine during open-heart surgery can result in complications such as cognitive changes or kidney impairment in some patients.
Furthermore, postoperative arrhythmias, including atrial fibrillation, are relatively common and may require additional interventions or long-term medication.
For patients receiving mechanical valves, the need for lifelong anticoagulation increases the risk of bleeding complications, while bioprosthetic valves may eventually deteriorate, necessitating future procedures.
Each patient's overall health, age, and comorbidities significantly influence these risks. As a result, thorough preoperative assessments and meticulous postoperative care are essential to minimize complications, ensuring that the life-saving benefits of aortic valve replacement are achieved while managing its potential hazards.
What are the types of Aortic valve surgery?
Aortic valve surgery encompasses several techniques designed to replace or repair a diseased aortic valve, each tailored to the patient's unique clinical needs.
The traditional method is open-heart surgery, which involves a full sternotomy to access the heart directly. During this procedure, the surgeon removes the faulty valve and implants a prosthetic valve—either mechanical or bioprosthetic.
Mechanical valves offer durability but require lifelong anticoagulation, while bioprosthetic valves, typically made from animal tissue, tend to have a shorter lifespan and usually do not require long-term blood thinners.
In recent years, minimally invasive techniques have advanced the field significantly. Transcatheter Aortic Valve Replacement (TAVR), for instance, involves threading a catheter—usually through the femoral artery—to deliver and deploy a new valve inside the diseased one, all without the need for open-heart surgery. This approach is particularly beneficial for older patients or those considered high-risk for conventional surgery.
Additionally, evolving surgical methods include minimally invasive incisions and rapid deployment valves, which reduce operative time and recovery duration. Each approach is determined based on factors such as the patient's age, overall health, and severity of the valve condition, ensuring that every patient receives a personalized treatment plan that balances procedural risk with long-term outcomes.
What is the surgery process of Aortic valve replacement?
Aortic valve replacement surgery follows a multi-stage process designed to restore healthy heart function. Prior to the procedure, patients undergo comprehensive evaluations—including imaging studies, blood tests, and risk assessments—to confirm they are suitable candidates.
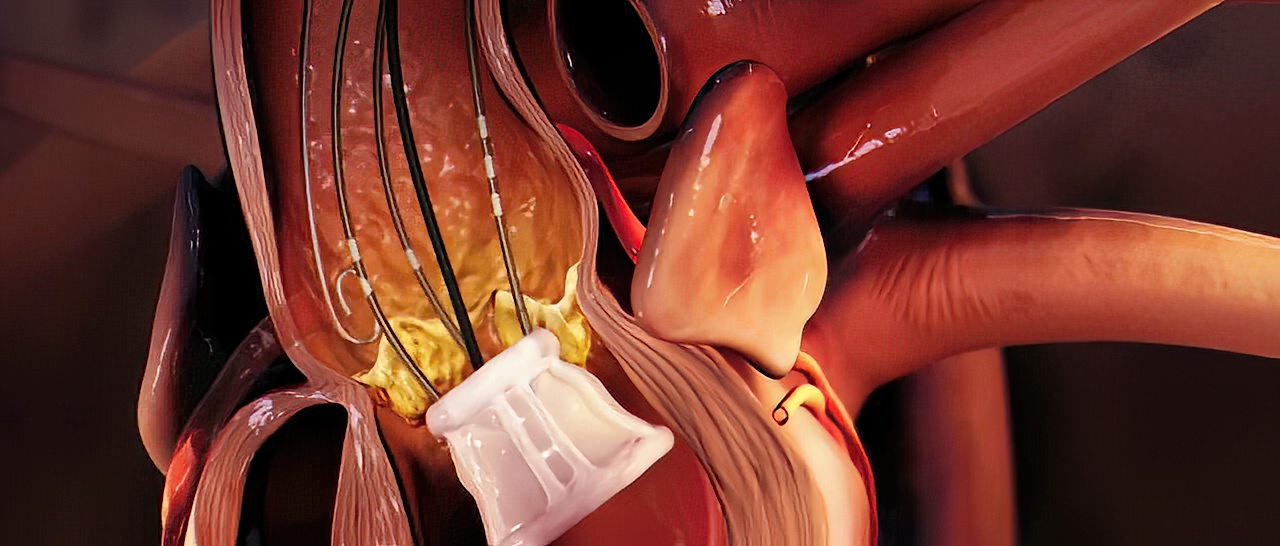
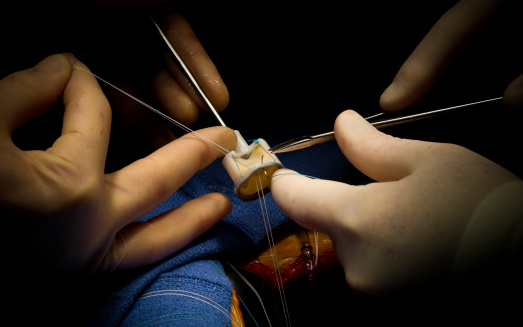
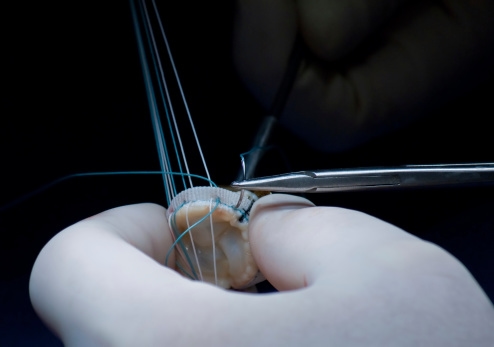
On the day of surgery, the patient is given general anesthesia, and the surgical team makes an incision in the chest, typically through a sternotomy, to gain access to the heart. Once the heart is exposed, a heart-lung bypass machine temporarily takes over the functions of the heart and lungs, ensuring oxygenated blood circulates throughout the body while the heart is temporarily stopped. The surgeon carefully removes the diseased or malfunctioning aortic valve and prepares the area for the new valve. Depending on individual needs, the replacement valve, which may be mechanical for durability or bioprosthetic for a more natural option with less need for long-term blood thinners, is then securely sewn into place.
After successful implantation, the heart is restarted and the bypass machine is gradually discontinued as normal circulation resumes. Finally, the chest is closed with sutures or staples, and the patient is transferred to an intensive care unit for close monitoring during the immediate postoperative period. This meticulous process helps restore proper blood flow, improving cardiac function and enhancing long-term quality of life.
Conclusion
Aortic valve replacement surgery stands as a transformative intervention in the management of advanced valve disease, offering renewed hope and restored quality of life for countless patients. This procedure, addresses the critical issues of reduced blood flow and cardiac strain caused by conditions such as aortic stenosis or regurgitation. The surgery involves meticulous planning, advanced surgical techniques, and comprehensive postoperative care to minimize risks such as infection, bleeding, or arrhythmias, which underscores its complexity and the high level of expertise required. Nonetheless, the benefits—ranging from symptom relief to improved cardiovascular efficiency and extended survival—are profound. With ongoing advancements in surgical technology and patient management practices, the procedure continues to evolve, becoming safer and more accessible to a broader patient population.
Read More