Tympanoplastyis a surgical procedure to repair a perforated eardrum (tympanic membrane) or the small bones of the middle ear. There are several types of tympanoplasty surgeries, each tailored to the specific needs of the patient.
What is Tympanoplasty?
Tympanoplastyprocedure is often necessary when the eardrum has been damaged due to chronic ear infections, trauma, or other medical conditions that affect the ear’s structure and function. The primary goal of tympanoplasty is to restore the integrity of the eardrum and improve hearing by reconstructing the sound conduction pathway.
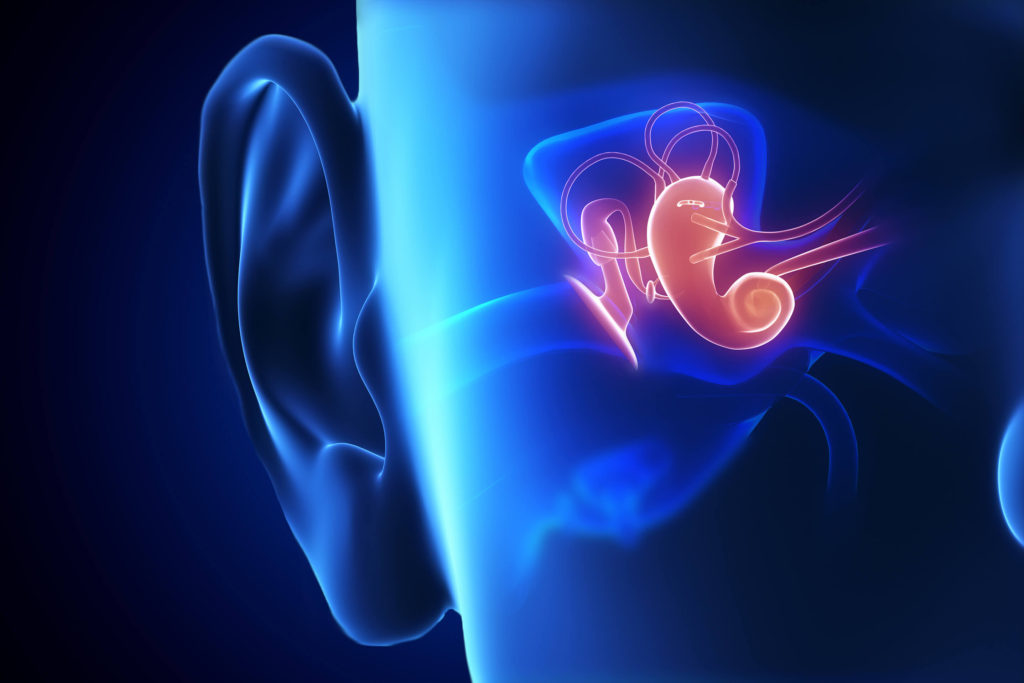
The eardrum plays a crucial role in hearing by vibrating in response to sound waves and transmitting these vibrations to the small bones (ossicles) in the middle ear. When the eardrum is perforated, it can lead to hearing loss, recurrent ear infections, and discomfort. Tympanoplasty addresses these issues by using a graft, typically made from the patient’s own tissue, to close the perforation and restore the eardrum’s functionality.
There are several types of tympanoplasty, each tailored to the specific needs of the patient. The choice of tympanoplasty type depends on the extent of the damage and the specific needs of the patient. The procedure is typically performed under general anesthesia, and the recovery period can vary depending on the complexity of the surgery. Patients may experience some discomfort and temporary hearing loss during the healing process, but the long-term benefits of improved hearing and reduced risk of infections make tympanoplasty a valuable intervention for those with eardrum perforations.

Types & classifications of Tympanoplasty
The classification of tympanoplasty is based on the extent of damage to the ear structures and the specific surgical techniques used to address these issues. There are five main types of tympanoplasty, each designed to address different levels of damage and restore hearing as effectively as possible; including:
Type I Tympanoplasty (Myringoplasty)is the simplest form of the procedure and focuses solely on repairing small perforations in the eardrum without involving the ossicles (the small bones in the middle ear). In this type, a graft, usually made from the patient’s own tissue, is placed over the perforation to allow the eardrum to heal and restore its functionality. This type is typically used when the ossicles are intact and functioning properly.
Type II Tympanoplastyis used when the perforation extends to the malleus, one of the ossicles. In this procedure, the graft is placed on the incus, another ossicle, to re-establish the connection between the eardrum and the inner ear. This type of tympanoplasty is necessary when the malleus is damaged or missing, but the incus and stapes (the other two ossicles) are still functional.
Type III Tympanoplastyaddresses damage to both the eardrum and the malleus and incus. In this procedure, the graft is placed directly on the stapes, the third ossicle, to re-establish the sound conduction pathway. This type is used when both the malleus and incus are damaged or missing, but the stapes is still functional.
Each type of tympanoplasty is designed to address different levels of damage and restore hearing as effectively as possible. The choice of procedure depends on the extent of the damage and the specific needs of the patient. Tympanoplasty is typically performed under general anesthesia, and the recovery period can vary depending on the complexity of the surgery.
Most common grafts used in Tympanoplasty
One of the critical components of this procedure is the graft material used to close the perforation and restore the integrity of the eardrum. The choice of graft material can significantly impact the success of the surgery and the patient’s recovery. Several types of grafts are commonly used in tympanoplasty, including:
Autologous Graftsare the most commonly used grafts in tympanoplasty. These grafts are harvested from the patient’s own body, which reduces the risk of rejection and infection. The most frequently used autologous grafts include:
Temporalis Fascia:This is the most popular graft material for tympanoplasty. The temporalis fascia is a thin layer of connective tissue located above the ear. It is easily accessible, has excellent tensile strength, and integrates well with the eardrum tissue. The use of temporalis fascia results in high success rates and minimal complications.
Tragal Perichondrium:This graft is taken from the cartilage covering of the tragus, a small projection in front of the ear canal. Tragal perichondrium is robust and provides good support for the eardrum. It is particularly useful in cases where the perforation is large or the middle ear requires additional support.
Cartilage Grafts:Cartilage grafts, often harvested from the tragus or the conchal bowl (the outer ear), are used in cases where the eardrum requires additional rigidity. Cartilage is resistant to retraction and resorption, making it ideal for patients with recurrent perforations or eustachian tube dysfunction. Cartilage grafts can be used alone or in combination with other graft materials.
Allograftsare grafts obtained from a donor of the same species. These grafts are processed and sterilized to reduce the risk of infection and rejection. Allografts are less commonly used than autologous grafts but can be an option when autologous tissue is not available or suitable.
Xenograftsare grafts obtained from a different species, such as bovine or porcine tissue. These grafts are also processed and sterilized to ensure safety. Xenografts are rarely used in tympanoplasty due to the higher risk of rejection and complications compared to autologous and allografts.
Synthetic Graftsare man-made materials designed to mimic the properties of natural tissue. These grafts are used less frequently in tympanoplasty but can be an option in specific cases. Synthetic grafts offer the advantage of being readily available and free from the risk of disease transmission. However, they may not integrate as well with the natural tissue as autologous grafts.

Incision approaches for Tympanoplasty
The success of Tympanoplasty surgery depends not only on the choice of graft material but also on the incision approach used to access the middle ear. There are several incision approaches for tympanoplasty, each with its advantages and considerations. The choice of approach depends on the location and size of the perforation, the patient’s anatomy, and the surgeon’s preference.
Endaural Approach:The endaural approach involves making an incision within the ear canal. This approach provides direct access to the eardrum and middle ear structures without the need for an external incision. The endaural approach is particularly useful for small to medium-sized perforations and offers excellent cosmetic results since the incision is hidden within the ear canal.
Postauricular Approach:The postauricular approach involves making an incision behind the ear. This approach provides excellent exposure to the middle ear and allows the surgeon to work comfortably on larger perforations or when extensive reconstruction is needed. The postauricular approach is versatile and can be used for various types of tympanoplasty. The main drawback is the visible scar behind the ear, although it typically heals well and becomes less noticeable over time.
Transcanal Approach:The transcanal approach involves making an incision within the ear canal, similar to the endaural approach, but with a focus on using specialized instruments to access the middle ear through the canal. This approach is minimally invasive and offers good cosmetic results. It is suitable for small to medium-sized perforations and cases where minimal middle ear work is required.
The goal is to provide optimal access to the middle ear while minimizing trauma and ensuring good cosmetic results.

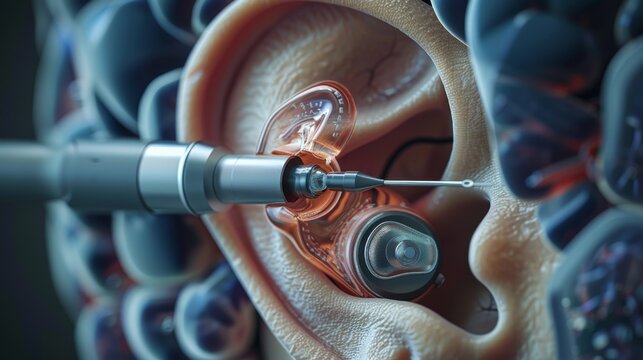
Techniques of placement of Graft in Tympanoplasty
One of the critical aspects of this procedure is the placement of the graft material to close the perforation and restore the integrity of the eardrum. The success of tympanoplasty largely depends on the precise and effective placement of the graft. Several techniques are commonly used for graft placement, including:
Underlay Technique:The underlay technique involves placing the graft material beneath the remaining eardrum and the edges of the perforation. This technique provides excellent support and stability for the graft, allowing it to integrate well with the existing eardrum tissue. The underlay technique is particularly useful for larger perforations and cases where the eardrum is retracted or atrophic. It offers a high success rate and is widely used in tympanoplasty procedures.
Overlay Technique:The overlay technique involves placing the graft material on top of the remaining eardrum and the edges of the perforation. This technique is beneficial for anterior perforations and cases where the eardrum is severely damaged or scarred. The overlay technique allows for precise placement of the graft and can result in excellent cosmetic outcomes.
Sandwich Technique:The sandwich technique combines elements of both the underlay and overlay techniques. In this approach, the graft material is placed both beneath and on top of the remaining eardrum, creating a “sandwich” effect. This technique provides additional support and stability for the graft, making it suitable for large or complex perforations.
Each technique for graft placement in tympanoplasty has its advantages and considerations. The choice of technique depends on the size and location of the perforation, the condition of the remaining eardrum, and the surgeon’s preference.
Conclusion
In conclusion, tympanoplasty surgery encompasses a range of procedures designed to repair perforations in the eardrum and address damage to the small bones of the middle ear. The classification into five types—Type I (Myringoplasty), Type II, Type III, Type IV, and Type V—allows for a tailored approach to each patient’s specific needs. Each type addresses different levels of damage, from simple eardrum perforations to more complex cases involving the ossicles. The choice of procedure depends on the extent of the damage and the patient’s unique anatomy, ensuring the most effective restoration of hearing and overall ear health. Tympanoplasty remains a vital intervention for improving the quality of life for individuals with eardrum perforations, offering long-term benefits of enhanced hearing and reduced risk of infections.
Read More