Pelvic floor reconstruction is a surgical approach designed to restore the structure and function of the pelvic floor, a group of muscles, ligaments, and connective tissues that support vital organs like the bladder, uterus, and rectum. This procedure is often recommended for individuals experiencing pelvic organ prolapse, a condition where weakened or damaged pelvic floor muscles cause organs to shift from their normal positions.
What is Pelvic Floor Reconstruction?
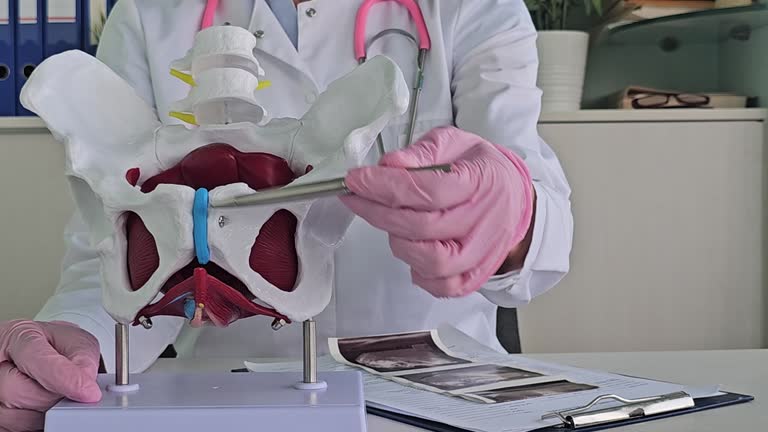
Pelvic floor reconstruction is a specialized surgical procedure designed to restore the structure and functionality of the pelvic floor, which is a complex network of muscles, ligaments, and connective tissues that support pelvic organs such as the bladder, uterus, vagina, and rectum. This procedure is commonly performed to address pelvic organ prolapse, a condition where weakened or damaged pelvic floor tissues result in the downward displacement of one or more pelvic organs. Pelvic organ prolapse often causes symptoms such as a feeling of heaviness or pressure in the pelvic area, urinary or bowel dysfunction, discomfort during physical activity, and, in severe cases, visible bulging of organs through the vaginal or rectal opening.
Pelvic floor reconstruction aims to reposition and stabilize the prolapsed organs while reinforcing the weakened support structures. The procedure is tailored to the patient's specific condition and the type of prolapse they are experiencing, such as uterine prolapse, vaginal vault prolapse, cystocele (bladder prolapse), rectocele (rectum prolapse), or enterocele (small intestine prolapse). Depending on the severity of the prolapse, pelvic floor reconstruction may involve the use of sutures, synthetic mesh, or biological grafts to strengthen the pelvic floor. In some cases, minimally invasive techniques like laparoscopic or robotic-assisted surgery are employed, providing greater precision, reduced tissue trauma, and faster recovery times.
The surgery can be performed through various approaches, including vaginal, abdominal, or laparoscopic access, depending on the location and complexity of the prolapse. For patients who no longer wish to have children or require additional interventions, pelvic floor reconstruction may be combined with other procedures, such as hysterectomy, to remove the uterus. Surgeons carefully assess each individual’s medical history, symptoms, and lifestyle factors to develop a personalized treatment plan.
Post-surgical recovery typically involves a period of rest and activity restrictions to allow proper healing. Patients may be advised to perform pelvic floor exercises, such as Kegel exercises, to strengthen the muscles and maintain long-term pelvic health. Pelvic floor reconstruction not only resolves functional problems but also significantly improves quality of life by alleviating discomfort, restoring normal organ positioning, and enabling patients to resume daily activities with confidence.

Why is Pelvic Floor Reconstruction done?
Pelvic floor reconstruction is performed to address pelvic organ prolapse, a condition where thepelvic floormuscles and connective tissues weaken, causing one or more pelvic organs—such as the bladder, uterus, rectum, or small intestine—to descend from their normal position. This condition can arise from various factors, including childbirth, aging, hormonal changes during menopause, obesity, chronic constipation, or repetitive heavy lifting. Pelvic organ prolapse can lead to symptoms such as pelvic pressure, discomfort, urinary incontinence, difficulty with bowel movements, and, in severe cases, visible protrusion of pelvic organs through the vaginal or rectal opening. These symptoms not only cause physical discomfort but can also significantly impact a person’s emotional well-being, self-confidence, and ability to engage in daily activities.
The primary objective of pelvic floor reconstruction is to restore the structure and function of the pelvic floor, alleviating symptoms and improving quality of life. This procedure is particularly recommended for individuals whose prolapse causes persistent discomfort or disrupts urinary, bowel, or sexual function, especially when non-surgical options such as pelvic floor exercises, pessary devices, or lifestyle modifications fail to provide sufficient relief. By repositioning and securing the prolapsed organs and reinforcing the weakened support structures, pelvic floor reconstruction addresses the root cause of the problem, providing long-term relief from symptoms and preventing recurrence.
Additionally, pelvic floor reconstruction is tailored to the specific type and severity of prolapse each patient experiences. For example, cystocele (bladder prolapse), rectocele (rectum prolapse), uterine prolapse, or vaginal vault prolapse may require different surgical approaches. The surgery not only relieves physical discomfort but also resolves functional impairments, enabling patients to regain control over their urinary and bowel functions, participate more actively in physical activities, and improve their overall sense of well-being. It also has a positive impact on intimate relationships by addressing discomfort during intercourse, restoring confidence, and enhancing quality of life.
Who would need a Pelvic Floor Reconstruction?
Pelvic floor reconstruction is typically recommended for individuals experiencing pelvic organ prolapse, a condition where the muscles, ligaments, and connective tissues of the pelvic floor weaken, causing organs such as the bladder, uterus, rectum, or small intestine to shift out of their normal position. This procedure is often necessary for those whose prolapse significantly affects their quality of life by causing physical discomfort or functional impairments. Common symptoms indicating the need for pelvic floor reconstruction include a sensation of heaviness or pressure in the pelvic area, urinary incontinence, difficulty emptying the bladder or bowels, and discomfort during physical activity or sexual intercourse. In severe cases, patients may notice a visible bulge or protrusion of pelvic organs through the vaginal or rectal opening, which can interfere with daily activities and overall well-being.
Individuals most likely to requirepelvic floor reconstructionoften have risk factors that predispose them to prolapse. These include women who have undergone multiple vaginal deliveries, as childbirth can place significant strain on the pelvic floor muscles and connective tissues. Other contributing factors include aging, hormonal changes during menopause that weaken tissues, obesity, chronic constipation, persistent heavy lifting, or prior pelvic surgeries. Additionally, genetic predispositions to weakened connective tissues can increase the likelihood of developing pelvic organ prolapse, making surgery a necessary option for some individuals.
Candidates for pelvic floor reconstruction are often those who have not found sufficient relief through non-surgical interventions, such as pelvic floor exercises, physical therapy, or the use of a pessary device. While these options can be effective for mild cases, individuals with moderate to severe prolapse or persistent symptoms may require surgical intervention to restore the pelvic floor’s structure and function. Pelvic floor reconstruction is also considered for those who wish to regain mobility, confidence, and the ability to engage in physical and social activities without the limitations caused by prolapse-related discomfort.

Types of pelvic reconstructive surgeries
Pelvic reconstruction surgeries are tailored to address pelvic organ prolapse by restoring the structure and function of the pelvic floor. Several types of surgeries are available, each suited to specific conditions and patient needs.
Native tissue repairis a common approach that uses the patient’s own tissues to reinforce and support the prolapsed organs. During this procedure, the surgeon stitches the prolapsed organs to the pelvic muscles or ligaments, repositioning them to their correct anatomical location. This method avoids the use of synthetic materials and is often recommended for patients with mild to moderate prolapse or those who prefer a natural repair.
Colporrhaphyis another widely used technique, particularly for anterior or posterior vaginal prolapse. In this procedure, the surgeon tightens the vaginal walls by stitching the connective tissues, providing better support for the bladder (anterior colporrhaphy) or rectum (posterior colporrhaphy). This surgery is typically performed through a vaginal approach and is effective in alleviating symptoms like urinary incontinence or bowel dysfunction caused by prolapse.
Sacrocolpopexyis a more advanced procedure often used for severe cases of vaginal vault prolapse. This surgery involves attaching a surgical mesh to the vaginal walls and securing it to the sacrum (tailbone) to provide long-lasting support. Sacrocolpopexy can be performed through open abdominal surgery or minimally invasive techniques like laparoscopy or robotic-assisted surgery. The use of mesh in this procedure ensures durability and reduces the risk of recurrence, making it a preferred option for many patients.
Each type of pelvic reconstruction surgery has its advantages and considerations, and the choice depends on the severity of the prolapse, patient preferences, and overall health. Consulting with a skilled surgeon is essential to determine the most appropriate approach for achieving optimal outcomes and improving quality of life.

What are the risks of Pelvic Floor Reconstruction?
Pelvic floor reconstruction, while generally safe and effective, carries certain risks and potential complications that patients should be aware of before undergoing the procedure.
One of the most common risks is bleeding, which can occur during or after surgery. In rare cases, excessive bleeding may require additional medical intervention.
Infection is another potential complication, as the surgical site is in a sensitive area. Proper post-operative care, including the use of prescribed antibiotics and maintaining hygiene, is crucial to minimizing this risk. Some patients may experience pain or discomfort during the recovery period, which is typically managed with medications and gradually subsides over time.
Another risk associated with pelvic floor reconstruction is damage to surrounding organs or tissues, such as the bladder, rectum, or urethra, due to the close proximity of these structures to the surgical site. This can lead to complications like urinary or bowel dysfunction, which may require further treatment.
In cases where synthetic mesh is used, there is a risk of mesh erosion or exposure, which can cause discomfort, infection, or the need for additional surgery to remove or replace the mesh. Although advancements in surgical techniques have reduced the likelihood of these issues, they remain a consideration for some patients.

Pelvic Floor Reconstruction procedure recovery
The recovery process following pelvic floor reconstruction is crucial to ensure proper healing and long-term success of the procedure. Most patients can return home the same day or within 24 hours after surgery, depending on the complexity of the operation and the surgical approach used. In the first few days post-surgery, patients may experience mild discomfort, swelling, or soreness in the pelvic area. These symptoms are typically managed with prescribed pain medications and rest. Some individuals may also have temporary urinary or bowel changes, which usually resolve as the body adjusts to the reconstructed pelvic floor.
Activity restrictions are an essential part of recovery. Patients are advised to avoid heavy lifting, vigorous exercise, or straining for several weeks to prevent undue pressure on the surgical site. Gradual light activity, such as short walks, helps promote circulation and reduces the risk of blood clots, which can occur after surgery. In many cases, doctors recommend elevating the legs and sleeping with the pelvis supported to minimize swelling. For patients who have undergone procedures involving mesh, additional care is taken to monitor healing and ensure the mesh integrates well with the surrounding tissues.
Follow-up visits with the surgeon are scheduled within the first week to assess the healing progress and address any concerns. During these appointments, the surgeon may remove any temporary devices, such as vaginal packing or catheters, if they were placed during surgery. Patients are also instructed to perform pelvic floor exercises, such as Kegels, once cleared by their doctor, as these exercises strengthen the muscles and reduce the likelihood of future prolapse. Proper hydration and maintaining a fiber-rich diet are recommended to prevent constipation, which can strain the pelvic floor and hinder recovery.
While most patients notice improvements in their symptoms within weeks, full recovery typically takes about six weeks to several months, depending on the extent of the surgery and individual factors like age and overall health. It is important to follow all post-operative guidelines and communicate with healthcare providers about any unusual symptoms, such as excessive bleeding, fever, or persistent discomfort. With proper care, pelvic floor reconstruction offers significant relief from prolapse-related symptoms and improves quality of life, enabling patients to resume their daily activities and regain confidence.

Conclusion
Pelvic floor reconstruction is a transformative surgical solution for individuals experiencing the challenges of pelvic organ prolapse. By restoring the structural integrity and functionality of the pelvic floor, this procedure alleviates discomfort, enhances urinary and bowel control, and improves overall quality of life. Tailored to meet the specific needs of each patient, pelvic floor reconstruction employs various advanced techniques, including native tissue repair, colporrhaphy, and minimally invasive approaches like sacrocolpopexy. Although the procedure carries some risks, careful surgical planning, adherence to post-operative guidelines, and ongoing communication with healthcare providers significantly minimize complications. For those with severe prolapse, this surgery offers a lasting resolution to a condition that can deeply impact daily activities, physical comfort, and self-confidence.
Read More