Gastrectomy is a major surgical intervention that involves removing a portion—or in some cases, the entirety—of the stomach to address serious gastrointestinal conditions.
What is Gastrectomy surgery?
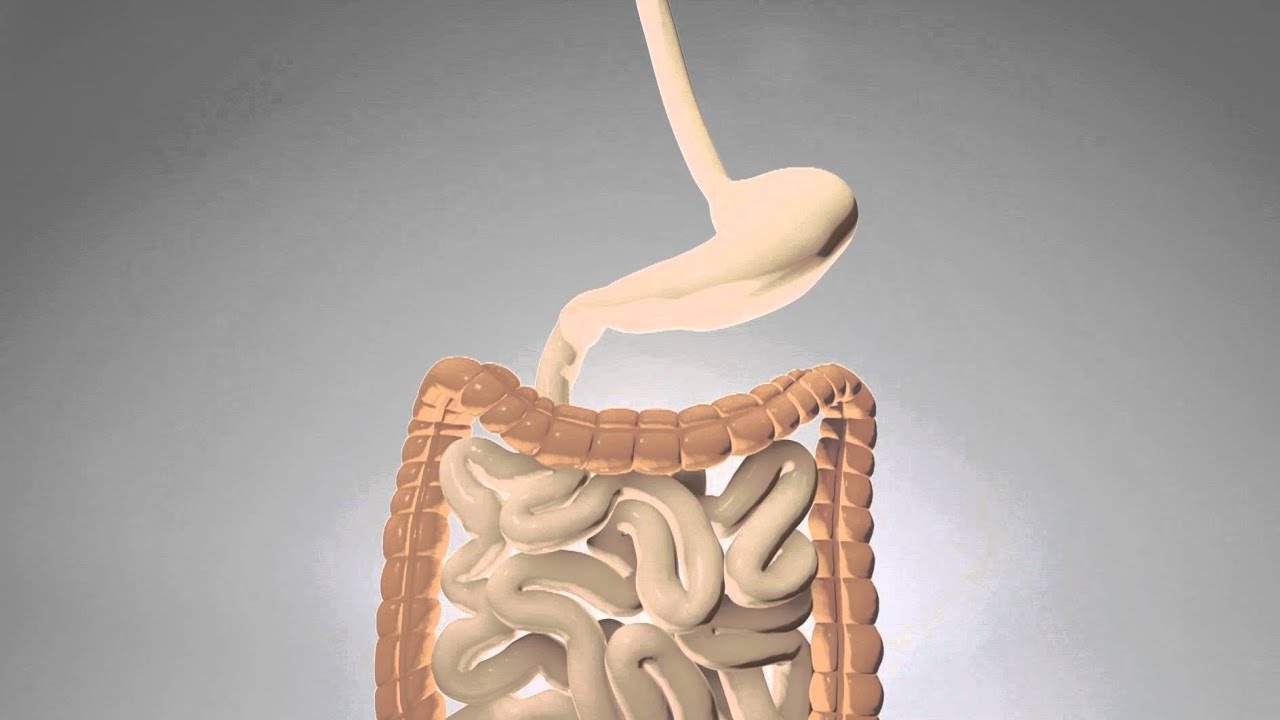
Gastrectomysurgery is a significant medical procedure that involves the removal of a portion or the entirety of the stomach to treat seriousgastrointestinal conditions. Typically recommended for patients with gastric cancer, severe peptic ulcers, benign tumors, or other debilitating stomach disorders, the surgery aims to eliminate diseased tissue and restore a functional digestive tract. Depending on the extent and location of the pathology, surgeons may perform a partial gastrectomy—removing only the affected segment—or a total gastrectomy, which entails the complete removal of the stomach followed by reconstruction of the gastrointestinal tract to connect the esophagus directly to the small intestine. Modern advancements in surgical techniques, such as laparoscopic and robotic-assisted approaches, have made these procedures less invasive, reduced postoperative discomfort, and shortened recovery times. Comprehensive preoperative evaluations are essential to plan the surgery and minimize risks, while meticulous postoperative care, including dietary modifications and nutritional support, is crucial for successful healing. Overall, gastrectomy surgery not only addresses life-threatening or chronic gastric conditions but also significantly improves patient quality of life by restoring digestive functionality and enhancing long-term health outcomes.
What does each types of Gastrectomy treat?
Gastrectomy surgery comprises various types tailored to treat different gastric conditions based on the extent and location of disease.
Total gastrectomy, involving the complete removal of the stomach, is typically indicated for widespread gastric cancer or severe diffuse conditions, where eliminating all potentially affected tissue is crucial.
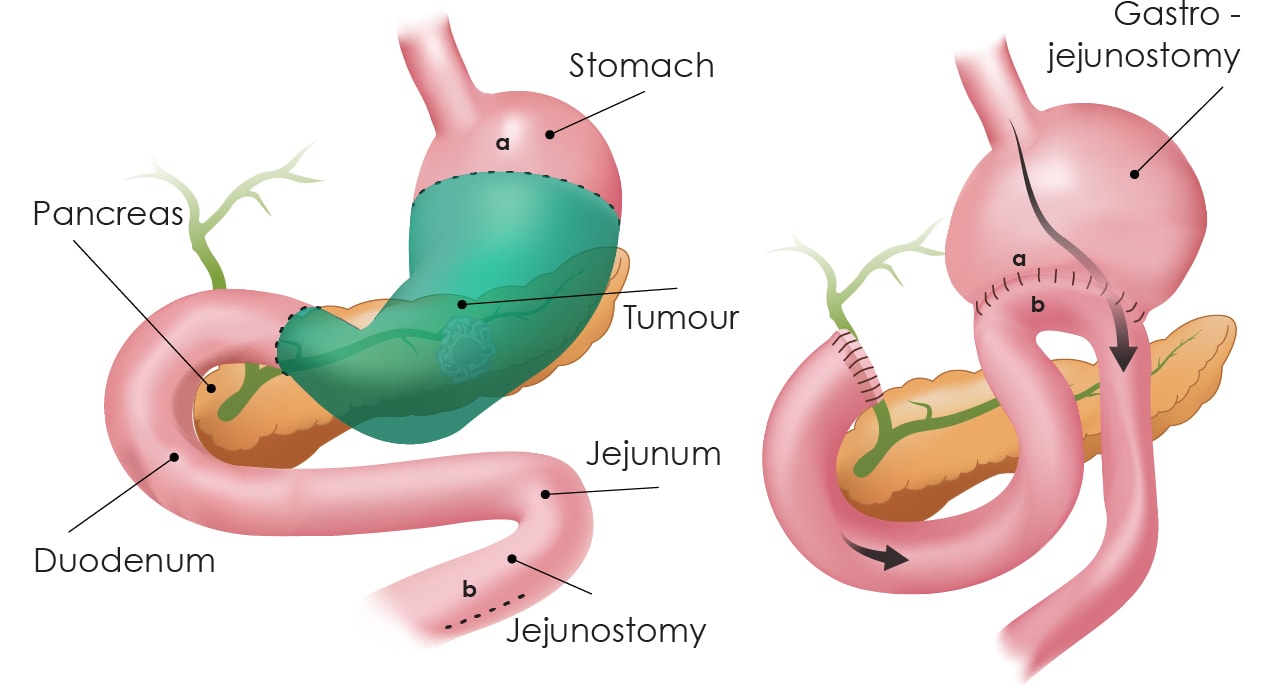
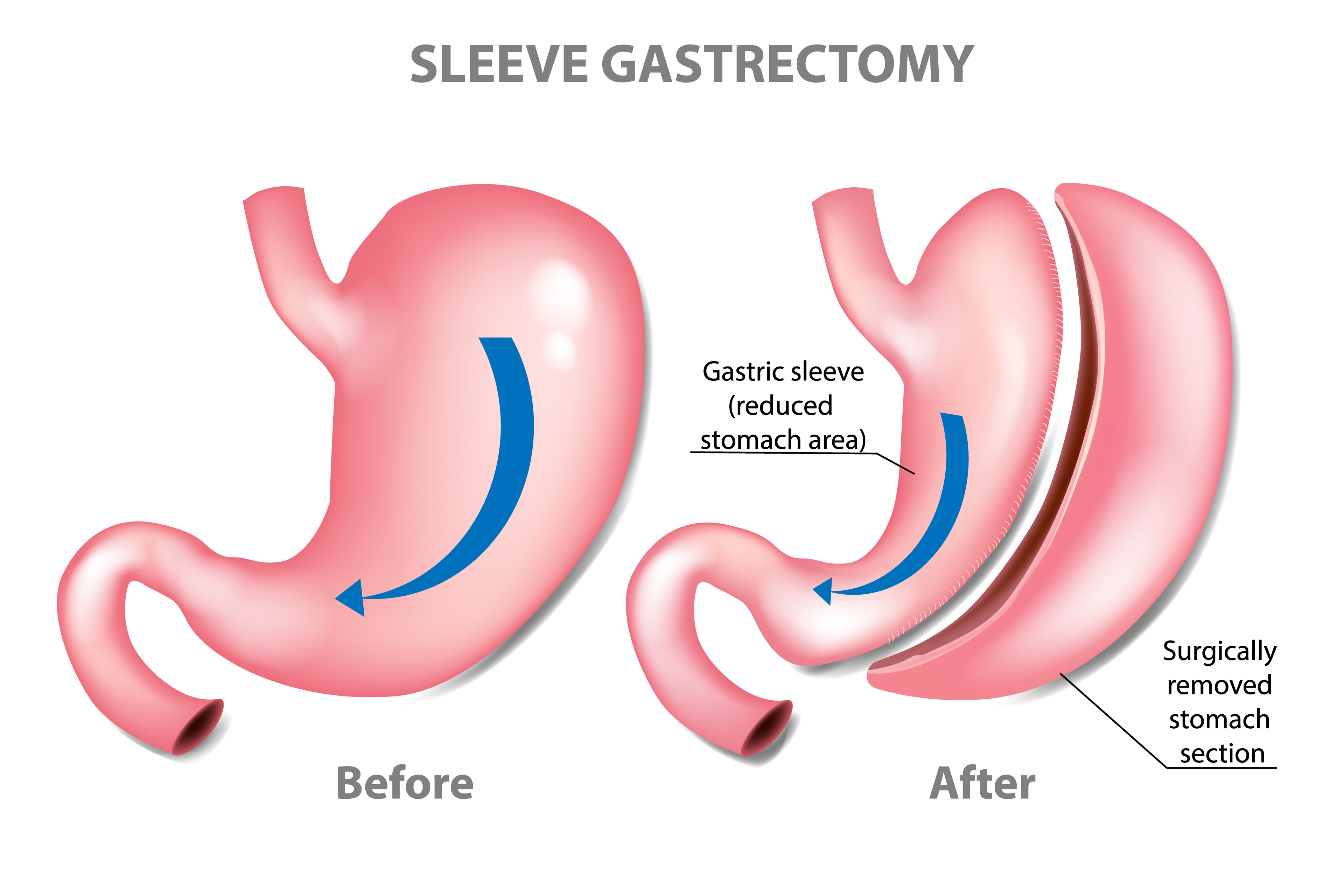
Partial, or subtotal, gastrectomy removes only a portion of the stomach and is commonly used when tumors, ulcers, or benign lesions are localized to a specific region, offering effective treatment while preserving some gastric function.
Distal gastrectomy, which excises the lower part of the stomach, is frequently employed to manage cancers or ulcerative conditions situated near the pyloric end, ensuring comprehensive resection and symptom relief.
In contrast, proximal gastrectomy, focused on removing the upper stomach, is often chosen when disease is confined to the cardia or near the gastroesophageal junction, thereby minimizing surgical impact on remaining gastric anatomy.
Each gastrectomy type is carefully selected based on the pathology, tumor location, and patient-specific factors, ensuring personalized treatment plans that optimize outcomes and maintain quality of life.
What are alternative treatments to Gastrectomy?
While gastrectomy is the established treatment for certain gastric conditions, alternative treatment options offer less invasive approaches and may preserve more of the stomach’s natural function.
For early-stage gastric cancers or localized lesions, minimally invasive endoscopic techniques such as endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) allow for removal of abnormal tissue without the need for full-scale surgery. These methods reduce recovery time and maintain gastric anatomy, potentially improving post-procedure quality of life.
Additionally, for advanced cases, neo-adjuvant therapies like chemotherapy, radiation, or targeted immunotherapy can shrink tumors before any surgical intervention is considered, sometimes making less radical surgery feasible.
In some benign conditions or dysplastic lesions, careful monitoring combined with medical management—such as acid suppression therapy for severe ulcers—may obviate the need for gastrectomy altogether.
Tailoring the treatment plan depends on various factors including the stage and type of the disease, the overall health of the patient, and the anticipated impact on quality of life.
How is Gastrectomy procedure done?
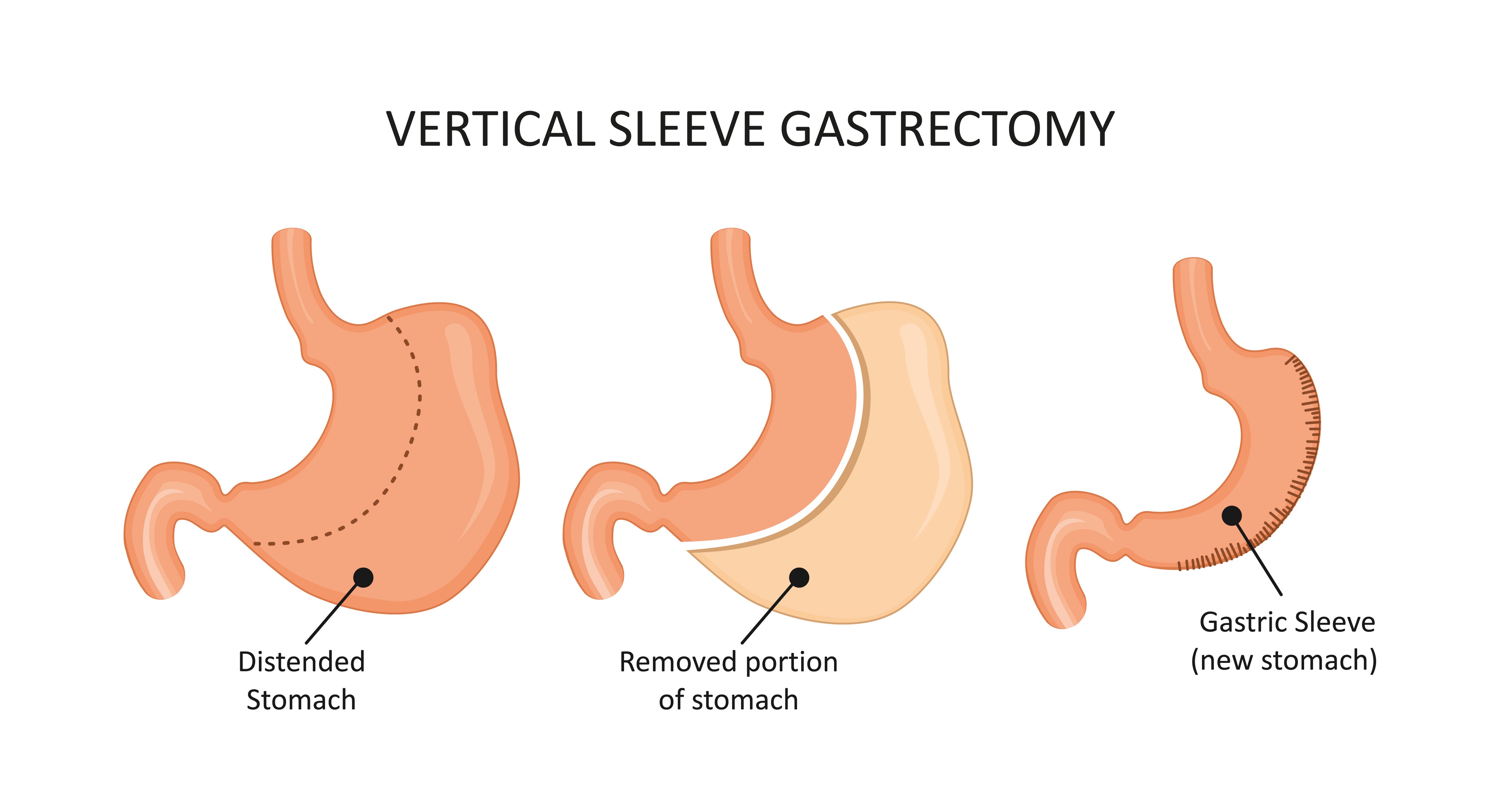
During a gastrectomy procedure, the patient is placed under general anesthesia to ensure complete unconsciousness and pain relief. The surgical team prepares the operating area in a sterile environment, and the procedure is performed either as an open surgery or using minimally invasive laparoscopic techniques. In an open gastrectomy, a large incision is made across the abdominal wall to provide the surgeon direct access to the stomach and adjacent organs. In the laparoscopic approach, several small incisions are used, through which a high-definition camera and specialized instruments are inserted to perform the surgery with greater precision and reduced recovery time. Once access is established, the surgeon carefully isolates the diseased portion of the stomach. For a partial gastrectomy, only the affected segment is removed; in a total gastrectomy, the entire stomach is excised. After removal, reconstruction of the gastrointestinal tract is performed, often using a Roux-En-Y anastomosis to reconnect the esophagus to the small intestine. Finally, the incisions are closed with sutures or staples, and post-operative care is initiated to monitor healing and ensure a smooth recovery. A highly experienced surgical team, utilizing the latest minimally invasive techniques, performs this operation with precision to optimize patient outcomes and ensure recovery.
Gastrectomy risks & benefits
Gastrectomy is a crucial surgical intervention for treating advanced gastrointestinal disorders, particularly gastric cancer and severe peptic ulcer disease.
This procedure offers considerable benefits, such as the complete removal of malignant or problematic tissues, significant alleviation of symptoms, and an overall improvement in quality of life. For many patients, gastrectomy eliminates chronic pain, bleeding, and obstruction issues that interfere with daily activities. In cases of localized disease, a partial gastrectomy can preserve digestive function while effectively addressing the pathology, whereas total gastrectomy with reconstructive techniques can still maintain nutritional continuity.
However, these benefits are counterbalanced by inherent risks. As a major operation, gastrectomy carries potential complications including postoperative infections, hemorrhage, and anastomotic leaks, which may require further medical intervention and extended hospitalization. Patients might also experience nutritional deficiencies, weight loss, and conditions such as dumping syndrome due to the altered digestion and reduced gastric capacity. Advances in minimally invasive surgical techniques, like laparoscopic or robotic-assisted procedures, have helped reduce recovery times and lower complication rates.
Ultimately, a thorough preoperative evaluation and comprehensive postoperative care are essential to managing these risks, ensuring that the substantial benefits of gastrectomy translate into optimal long-term patient outcomes.
Life after Gastrectomy
Life after gastrectomy represents a transformative period in which patients gradually adjust to a new normal. Most individuals are advised to adopt a modified diet that involves smaller, more frequent meals to ease digestion and minimize discomfort, such as symptoms associated with dumping syndrome. Since a significant portion of the stomach is removed, nutritional absorption can be altered, making regular monitoring and supplementation of vitamins and minerals—especially vitamin B12, iron, and calcium—an essential part of post-surgery care. Recovery involves both physical and emotional adjustment, as patients learn new eating habits and coping strategies for any digestive changes. Alongside dietary modifications, a tailored exercise regime, gentle physical activity, and consistent follow-ups with healthcare professionals contribute to enhanced overall well-being and prevent complications. Many patients find that with time, they experience increased energy levels and an improved quality of life, as the resolution of chronic stomach-related issues leads to less pain and a greater sense of freedom. Ongoing patient education, supportive counseling, and nutritional guidance help in managing long-term changes and optimizing recovery.
Conclusion
In conclusion, gastrectomy is a critical surgical intervention that not only addresses severe gastric conditions but also paves the way for improved quality of life. Although the procedure presents challenges such as significant dietary adjustments and the potential for nutritional deficiencies, advancements in surgical techniques and postoperative care have considerably enhanced patient outcomes. With either partial or total removal of the stomach, the primary goal is to eliminate disease while preserving quality of life through careful reconstruction and an individualized recovery plan. Ultimately, the success of gastrectomy relies on a well-coordinated approach that combines expert surgical care, thorough preoperative evaluation, and ongoing rehabilitation, ensuring that patients can confidently move toward a healthier, more active future.
Read More