Arrhythmia surgery is a specialized branch of cardiac care focused on correcting irregular heart rhythms that can compromise the heart’s efficiency and overall well-being.
Who needs Arrhythmia Surgery?
Arrhythmia surgeryis generally recommended for individuals whose irregular heart rhythms pose significant health risks or are unresponsive to conventional therapies. Typically, patients with persistent atrial fibrillation or other chronic arrhythmias that lead to debilitating symptoms—such as severe palpitations, breathlessness, chest pain, or fatigue—are considered potential candidates. This treatment becomes especially crucial when medications or less invasive procedures like catheter ablation have failed to restore a normal rhythm, or when there is a high risk of complications such as stroke or heart failure. Patients with ventricular arrhythmias, which can lead to sudden cardiac arrest, may also require surgical intervention to stabilize their condition and improve survival outcomes. Furthermore, individuals with structural heart abnormalities orcongenital heart defectsthat predispose them to complex arrhythmias might benefit from surgery as part of a broader treatment strategy aimed at improving overall cardiac function. In these cases, a thorough evaluation by a cardiologist and an electrophysiologist is essential to determine the potential benefits of surgery relative to the risks.

What are the types of arrhythmia?
Arrhythmias are abnormal heart rhythms that vary in their origin, speed, and clinical significance. Broadly, they fall into several categories based on heart rate and the site of origin.
One major category is bradyarrhythmias, characterized by a slower than normal heart rate, often resulting from dysfunction of the sinoatrial node or conduction blocks such as atrioventricular block.
In contrast, tachyarrhythmias are marked by an abnormally fast heart rate and are further subdivided into supraventricular and ventricular types.
Supraventricular arrhythmias originate in the heart's upper chambers and include common conditions like atrial fibrillation, in which chaotic electrical activity produces an irregular rhythm, and atrial flutter, presenting with a more regular yet rapid beat.
Paroxysmal supraventricular tachycardia also occurs in sudden, brief episodes of rapid heartbeat. Ventricular arrhythmias, such as ventricular tachycardia and ventricular fibrillation, are particularly serious due to their potential to impair the heart’s pumping ability and lead to life-threatening events.
These types of arrhythmias are diagnosed through various diagnostic tools and warrant tailored treatment to restore normal cardiac function and mitigate risks.

What are the warning signs of arrhythmia?
Arrhythmias, or irregular heart rhythms, can manifest through a diverse array of warning signs that may indicate an underlying issue with the heart's electrical system.
One of the most common indicators is palpitations—a sensation of fluttering, pounding, or skipping heartbeats that can alarm those experiencing it.
Many individuals also report episodes of dizziness or lightheadedness, often stemming from reduced blood flow to the brain during an arrhythmic event.
Shortness of breath, particularly when it occurs during routine activities or physical exertion, is another frequent symptom that suggests the heart is struggling to pump blood efficiently.
In addition, some people experience chest discomfort or pain, which may signal that the heart muscle is not receiving adequate oxygen.
Fatigue and a sudden, unexplained sense of weakness can also accompany arrhythmias, as the body copes with fluctuating cardiac output.
Recognizing these warning signals early is crucial, as they can be indicative of more serious conditions such as stroke or heart failure. Monitoring these symptoms and seeking prompt medical evaluation is essential for initiating timely treatment and preventing potential complications.
What are the risk factors for arrhythmia?
Arrhythmias—abnormal heart rhythms that can disrupt the heart’s natural pumping function—may develop from a combination of modifiable and non-modifiable risk factors.
Age is a major non-modifiable factor, as changes in the heart’s structure and conduction system over time increase susceptibility to irregular beats.
A family history of arrhythmia or other cardiac conditions further elevates the risk by predisposing individuals genetically.
Underlying cardiovascular problems such as coronary artery disease, heart failure, hypertension, and past heart attacks can damage the heart tissue, creating an environment prone to electrical disturbances.
In addition, conditions like diabetes, obesity, and thyroid imbalances can impair overall heart function, making arrhythmias more likely to occur.
Lifestyle choices also play a significant role—excessive alcohol consumption, high caffeine intake, smoking, and the use of illicit drugs can trigger or worsen abnormal rhythms.
Recognizing these risk factors is critical, as it enables individuals to make informed lifestyle adjustments and seek early medical intervention to reduce the likelihood of developing potentially life-threatening arrhythmias.

Why is surgery for arrhythmia necessary?
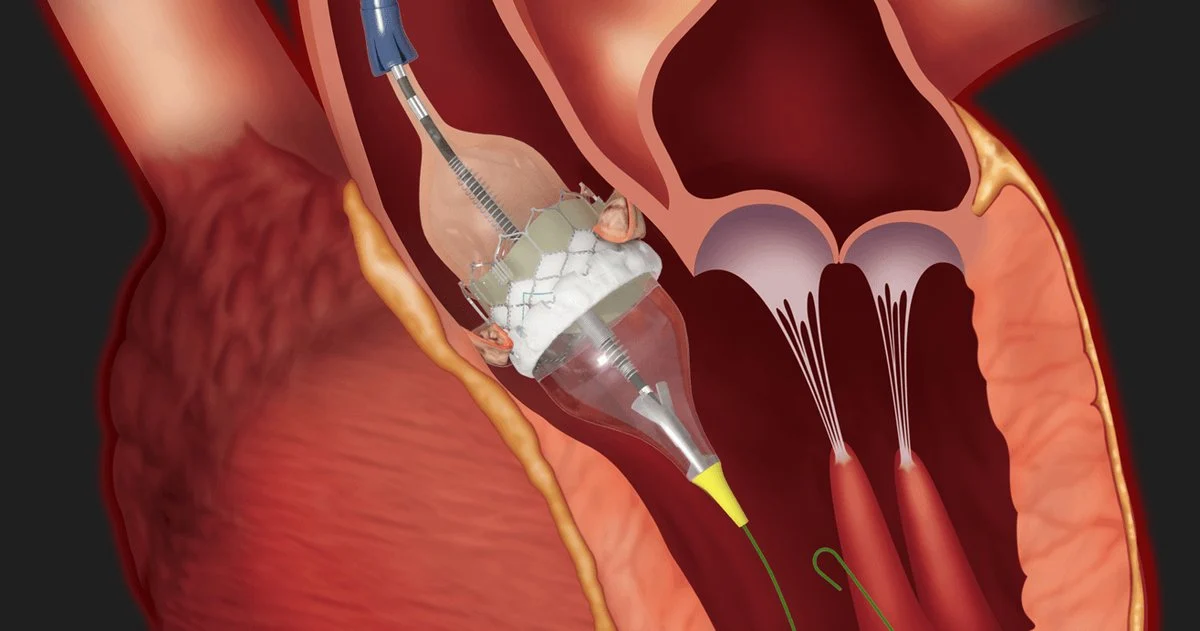
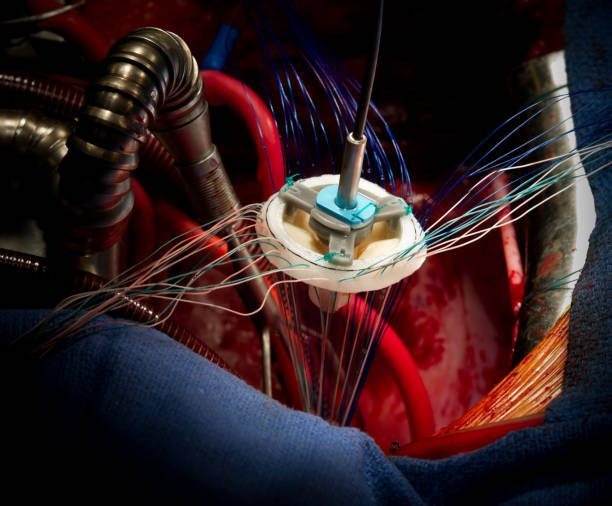
Arrhythmia surgery becomes necessary when irregular heart rhythms persist despite conventional treatments, posing significant health risks that compromise both cardiac function and quality of life. In many cases, medications and lifestyle modifications fail to adequately restore a stable heartbeat, leading to increased risks of stroke, heart failure, and sudden cardiac death. For patients with complex arrhythmias such as atrial fibrillation or ventricular tachycardia, surgical interventions like catheter ablation or the Maze procedure offer a targeted approach to eliminate the problematic tissue responsible for triggering abnormal electrical signals. Additionally, in cases where the heart’s conduction system is severely compromised, the implantation of devices such as pacemakers or defibrillators provides continuous monitoring and corrective therapy, mitigating the risk of life-threatening events. By directly addressing the source of the arrhythmia, surgery not only alleviates immediate symptoms but also contributes to long-term cardiac stability. This proactive intervention is essential for patients who have exhausted non-invasive treatment options, offering them renewed potential for a healthier, more active life. Ultimately, arrhythmia surgery plays a critical role in restoring normal heart function and protecting patients from further cardiac complications, improving both survival rates and overall well-being. Such surgery offers a lifeline for improved longevity and daily vitality.

Arrhythmia Surgery Recovery
Recovery from arrhythmia surgery requires careful management and time. Following the procedure, patients typically remain under close observation in a hospital setting to monitor vital signs, ensure the stability of heart rhythms, and manage any complications that might arise. The initial recovery phase often involves a period of rest while the body adjusts to the changes made during surgery. Patients may experience fatigue and mild discomfort, which gradually diminish with proper pain management and support. During the early weeks, doctors usually recommend limited physical activity to avoid placing undue stress on the heart. As recovery progresses, patients can gradually reintroduce light activities and participate in cardiac rehabilitation programs that encompass therapeutic exercise, stress management techniques, and nutritional counseling. Regular follow-up appointments are essential to track progress, adjust medications, and evaluate overall heart function. Emphasizing adequate rest, a balanced diet, and emotional support, a structured recovery plan not only restores physical strength but also nurtures psychological well-being. With adherence to medical advice and a gradual return to daily activities, most individuals eventually regain a regular lifestyle and enjoy an improved quality of life, marking a successful recovery from arrhythmia surgery.
Conclusion
Arrhythmia surgery stands as a critical intervention for patients whose irregular heart rhythms compromise their quality of life and pose serious health risks. This specialized branch of cardiac care brings together innovative techniques—ranging from catheter ablation and the Maze procedure to the implantation of pacemakers and defibrillators—to directly address the underlying causes of arrhythmias. While the decision to undergo surgery involves weighing potential risks against significant benefits, such as improved heart function and reduced risk of complications like stroke or heart failure, the evolution of surgical methods has continuously enhanced both safety and effectiveness. Patients who have exhausted less invasive treatments may find that surgery offers renewed hope through the restoration of a stable, regular heartbeat and the promise of a more active, fulfilling life.
Read More