Colon resection surgery, often referred to as colectomy, is a critical surgical procedure performed to remove a diseased or damaged portion of the colon.
What is a Colectomy?
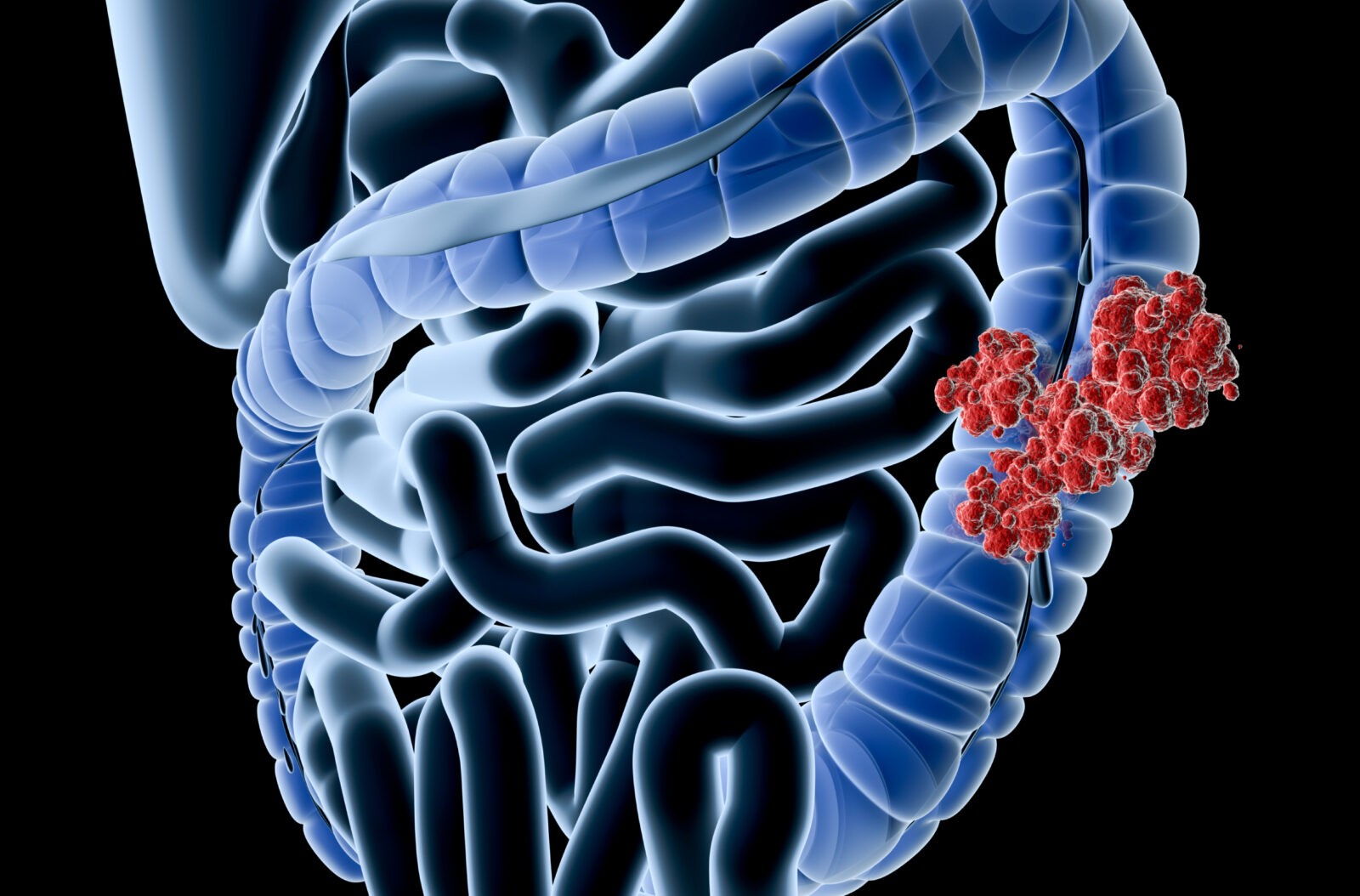
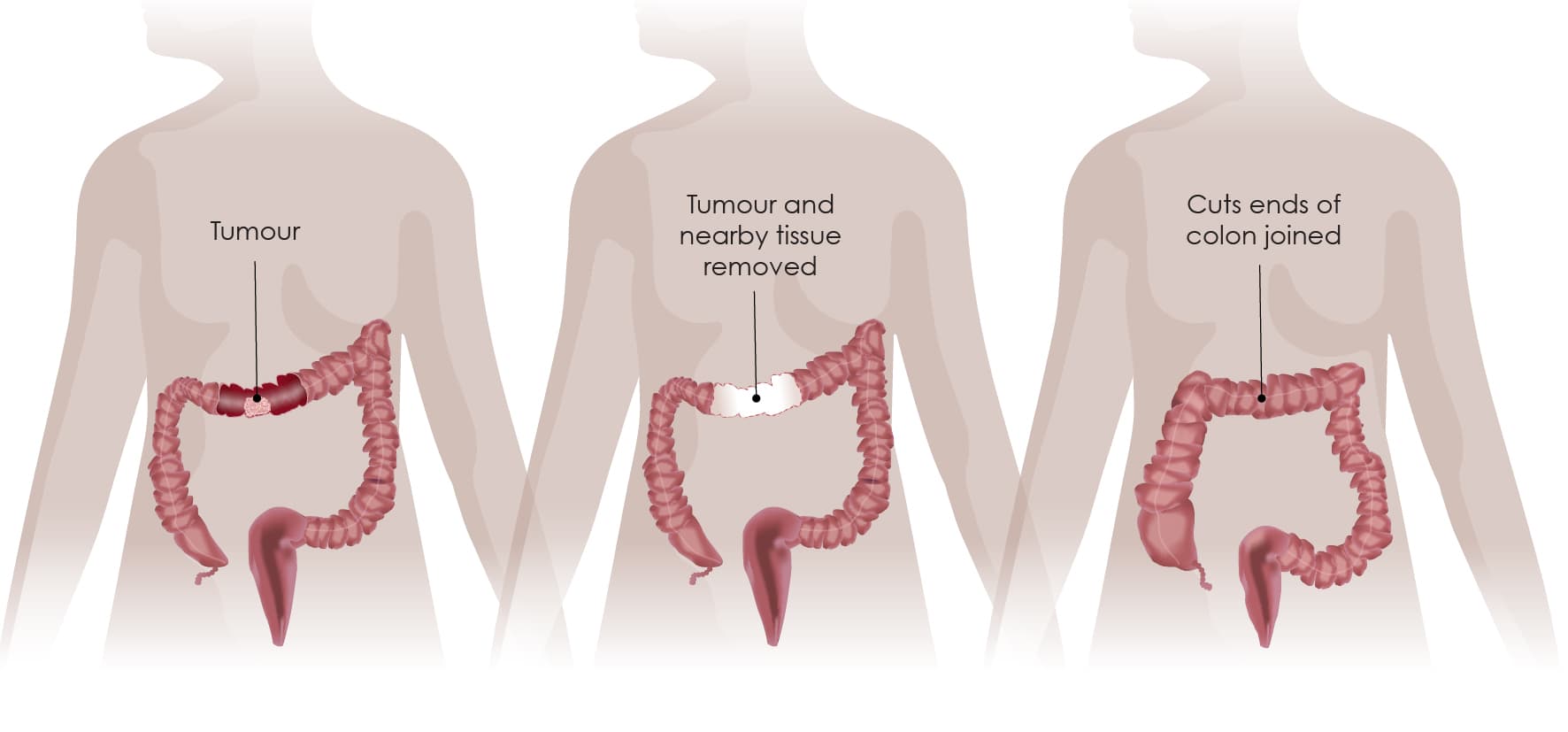
A colectomy is a surgical procedure that involves the partial or complete removal of thecolon, which is a vital component of the digestive system responsible for absorbing water and forming stool. This procedure is often indicated for patients suffering from serious conditions such as colon cancer, diverticulitis, inflammatory bowel disease (including Crohn’s disease and ulcerative colitis), or complicated cases of polyps and ischemic colitis. During acolectomy, the surgeon removes the affected portion of the colon and then reconnects the healthy sections through a process called anastomosis, allowing for the continuation of normal digestive functions. In some cases, when it is not possible to immediately reconnect the bowel, a colostomy or ileostomy may be created, which diverts waste to an external bag until further recovery can be achieved. Advances in surgical techniques have led to the adoption of minimally invasive methods like laparoscopic and robot-assisted colectomies, which typically result in reduced postoperative pain, shorter hospital stays, and faster recovery times compared to open surgery.
What are the types of Colectomy?
Colectomy is a versatile procedure with several subtypes tailored to address different segments of the colon and specific underlying conditions.
The main types include hemicolectomy, subtotal colectomy, and total colectomy, each differing in the extent of colon removal.
In a right hemicolectomy, the surgeon removes the ascending colon along with a portion of the transverse colon, whereas a left hemicolectomy involves excision of the descending colon and sometimes part of the sigmoid colon.
For conditions that affect a larger portion of the colon, a subtotal colectomy may be performed, preserving a segment of the colon while removing the majority of diseased tissue.
In more extensive cases, a total colectomy is undertaken, removing the entire colon and sometimes part of the rectum, especially in cases of familial polyposis or severe inflammatory bowel disease.
Additionally, modern surgical practices offer minimally invasive options such as laparoscopic and robotic-assisted colectomy, which yield reduced postoperative pain and faster recovery compared to open procedures.
The choice among these techniques depends on the patient’s diagnosis, overall health, and surgical risk, allowing for a more targeted, effective intervention that aims to restore gastrointestinal function and improve quality of life. Each technique is adapted to the patient’s specific needs.

How is a colectomy done?
A colectomy is performed under general anesthesia in a prepared operating room, following detailed preoperative evaluations. In a laparoscopic colectomy, the surgeon makes several small incisions in the abdomen to insert a laparoscope equipped with a camera for a magnified view of the colon. Specialized instruments are then introduced through additional incisions. The surgeon carefully identifies the diseased segment—whether affected by colon cancer, diverticulitis, inflammatory bowel disease, or polyps—and isolates it from healthy tissue. Once mobilized, the problematic portion is detached using surgical staples or sutures to safely seal blood vessels. The surgeon then reconnects the remaining healthy sections of the colon in a procedure known as anastomosis, restoring the continuity of the digestive tract. In certain cases, if immediate reconnection is not feasible, a temporary stoma (colostomy or ileostomy) may be created to allow healing before the bowel is reattached. Throughout the procedure, the surgical team monitors vital signs and manages any blood loss, ensuring patient safety. By employing minimally invasive techniques, colectomy offers benefits such as reduced postoperative pain, shorter hospital stays, and improved recovery times, ultimately enhancing the patient’s quality of life. This refined technique not only alleviates the underlying condition but also restores proper gastrointestinal function.
What are the risks of colon resection surgery?
Colon resection surgery, while often essential for treating serious bowel diseases, carries inherent risks that patients should understand prior to undergoing the procedure. The potential risks include both short-term complications and long-term challenges.
In the short term, patients may experience intraoperative complications such as bleeding, inadvertent injury to adjacent organs, or adverse reactions to anesthesia. Postoperatively, infection at the incision sites, deep vein thrombosis, pneumonia, and wound dehiscence are possible, particularly in those with preexisting health conditions. One of the most serious concerns is an anastomotic leak, where the surgical reconnection of the colon fails, leading to leakage of intestinal contents and potentially resulting in peritonitis—a life-threatening infection that might necessitate additional interventions.
Long-term risks include the development of adhesions that can cause bowel obstructions, and alterations in bowel habits, such as chronic diarrhea or constipation. There is also a potential for incisional hernias to develop years after surgery.
While advancements in minimally invasive techniques have reduced these risks, careful preoperative assessment and close postoperative monitoring remain crucial to mitigating complications and ensuring a successful recovery.
Colectomy recovery process
After a colectomy, the recovery process is a gradual journey toward restoring normal digestive function. Initially, patients remain hospitalized for several days while medical staff closely monitor vital signs, pain levels, and bowel movements. Early recovery involves starting on clear liquids followed by a slow progression to soft foods as digestion resumes, with pain medications and antibiotics helping manage discomfort and prevent infection. Rest and limited physical activity are crucial during the first week to allow healing, with gentle walking encouraged to improve circulation and reduce the risk of blood clots. As recovery progresses, personalized guidelines gradually reintroduce regular activities, including light exercise that aids muscle strength and coordination. Wound care instructions are vital to prevent complications such as infection or incisional hernias. Regular follow-up appointments ensure recovery remains on track and address any concerns during the healing process. Factors including the type of colectomy, overall health, and age influence the timeline, with some patients resuming normal routines within a few weeks and others requiring several months for full recovery.
Conclusion
In conclusion, colon resection surgery stands as a pivotal intervention in modern gastrointestinal medicine, offering both life-saving and quality-of-life-improving benefits for patients facing serious colonic diseases. By excising diseased or damaged segments of the colon, whether due to cancer, diverticulitis, inflammatory bowel disease, or other complications, this procedure addresses not only the immediate threat posed by the condition but also minimizes the risk of future complications. Advances in surgical methods, including laparoscopic and robotic-assisted techniques, have revolutionized colon resection by reducing trauma, shortening hospital stays, and enabling quicker recovery while minimizing scarring. Although no surgery is entirely without risk—such as potential infections, anastomotic leaks, or postoperative bowel irregularities—the careful assessment of each patient's medical history and comprehensive postoperative care are critical in mitigating these risks.
Read More